Most surgeries leave organs stuck together: New gel might prevent this


More elective surgeries will be cancelled across Australia ahead of an expected rush of patients with COVID-19. Photo: Getty
Stanford University researchers may have solved a common, sometimes fatal complication of surgery – simply known as adhesions.
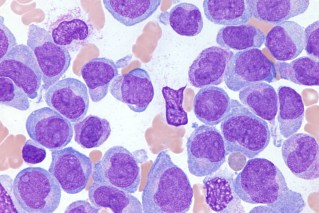
These are the fibrous bands that form between internal organs and tissues, sticking them together, as the surgical wounds heal.
Adhesions begin to form within the first few days after surgery – in 95 per cent of all cases – generally without causing problems.
Tricky and sticky business
But it’s tricky when they do, because they may not produce symptoms for months or even years – and there is no scan that can identify them.
A surgical procedure called adhesion lysis is the only way to remedy abdominal adhesions. They are otherwise permanent.
In the operation, the surgeon clips the fibres that have formed into adhesions and attempts to remove as much of this scar tissue as possible.
But inevitably, following this new surgery, more adhesions are bound to form.

The experimental gel was tried on sheep during heart surgery with great success. A sheep’s heart is about the size of a person’s heart. Photo: Getty
There is no reliable prevention.
You’re relying on your surgeon to minimise the risk of adhesions by using a gentle surgical technique and powder-free gloves.
For more than a century, surgeons have tried all manner of substances – including animal membranes, sheets of rubber and mineral oil – with limited success.
The Stanford researchers note that “current adhesion barriers approved by the Food and Drug Administration are rarely used; they are difficult to deploy and are considered ineffective.”
How bad can they be?
About 60 per cent of small bowel obstructions in adults are caused by adhesions: The blockages form when the scar tissue twists or compresses the intestines.
According to an explainer from Harvard University, sometimes an area of intestine that is affected by adhesions can keep becoming blocked then unblocked, causing symptoms to come and go.
Rarely, a portion of the bowel twists tightly around a band of adhesions.
This cuts off the normal blood supply to the twisted bowel, causing what is called “strangulation” and that section of bowel begins to die.
When this emergency happens, the person must be taken to surgery immediately.
“Adhesions are fairly rare in patients who have never had abdominal surgery. In people who have had multiple abdominal surgeries, adhesions are common,” says Harvard University.

Surgical adhesions are fibrous bands that form between organs and tissues during the natural healing process. Photo: Supplied
Adhesions are also believed to contribute to the development of chronic pelvic pain. Following gynaecological surgery, they can cause infertility.
Adhesions following heart surgery are especially problematic – especially when multiple surgeries are required.
As the authors note in their paper: “In cardiac surgery, pericardial adhesions are particularly problematic during re-operations, as surgeons must release the adhesions from the surface of the heart before the intended procedure can begin, thereby substantially lengthening operation times and introducing risks of haemorrhage and injury to the heart and lungs during sternal re-entry and cardiac dissection.”
So what’s the solution?
As with many promising scientific developments, the Stanford solution happened as a spontaneous “what if?” moment.
Lyndsay Stapleton, a graduate student in bioengineering, and lead author, was one day working with rats to develop an injectable therapy to reduce tissue damage following a heart attack,
Dr Eric Appel, an assistant professor of materials science and engineering – and a senior author of the paper – suggested that Ms Stapleton try spraying a polymer-nanoparticle hydrogel on to the rat hearts and surrounding tissue after surgery to see if it reduced the formation of adhesions.
Weeks later, when Ms Stapleton operated on the animals again, she saw that no adhesions had formed.
“It was pretty striking,” she said, in a prepared statement. “I thought, ‘Oh wow, we could be onto something here’.”
Success with rats and sheep, humans to follow
What followed was a study where the scientists formulated four additional gels with a range of properties.
After inducing heart attacks in rats, they randomly divided the animals into eight treatment groups: Five that each received a different gel, two that received commercially available adhesion barriers, and one that received no treatment.
Four weeks later, the rats that had received no treatment, or either of the two commercial adhesion barriers, had formed dense adhesions. Their hearts were connected to their chest walls.
The rats that were treated with two of the five gels had formed moderate to dense adhesions.
The rats treated with the other three gels fared much better, with very few adhesions.
However, the gel Stapleton initially tried – named PNP 1:10 – completely prevented adhesions.
The researchers then tested the gel in sheep, whose hearts are similar in size and shape to human hearts. They found similar results.
As part of the study, the researchers tested the rats to see if they showed any reaction to the gel; they saw no abnormalities in the surrounding tissues or in the blood.
The researchers next plan to try PNP 1:10 in abdominal surgery in rats.
They hope to conduct human trials soon.
“The difference between what we saw after using the gel and what we normally see after surgery was drastic,” said Joseph Woo, MD, professor and chair of cardio-thoracic surgery, and a senior author of the paper.